From medical imaging to 3D modelling
3D printing technique enables faster, better, and cheaper models of patient-specific medical data
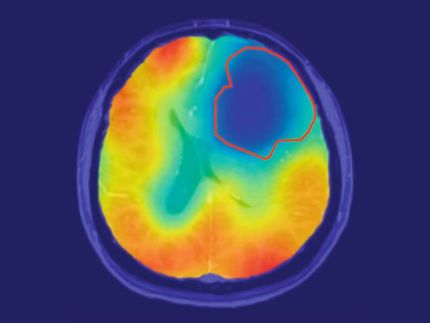
What if you could hold a physical model of your own brain in your hands, accurate down to its every unique fold? That question moved Steven Keating, Ph.D., who had a baseball-sized tumor removed from his brain at age 26 while he was a graduate student at the MIT. By collecting his imaging data he tried to reveal his former brain shape. This ended frustrating and he asked for help by former collaborators, that are exploring new 3D printing methods for biological samples.
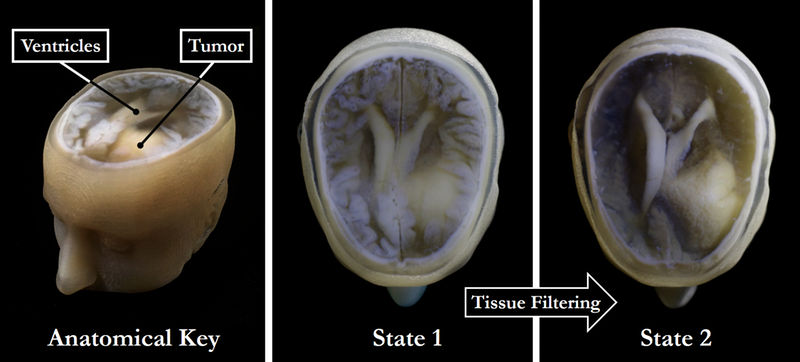
High-throughput tissue filtering, a major feature of the approach developed by the authors of the study, can help quickly remove extraneous tissues to reveal the desired underlying structures (right) without sacrificing the resolution or intensity gradients present in the native imaging data (left and center).
James Weaver and Steven Keating/Wyss Institute at Harvard University
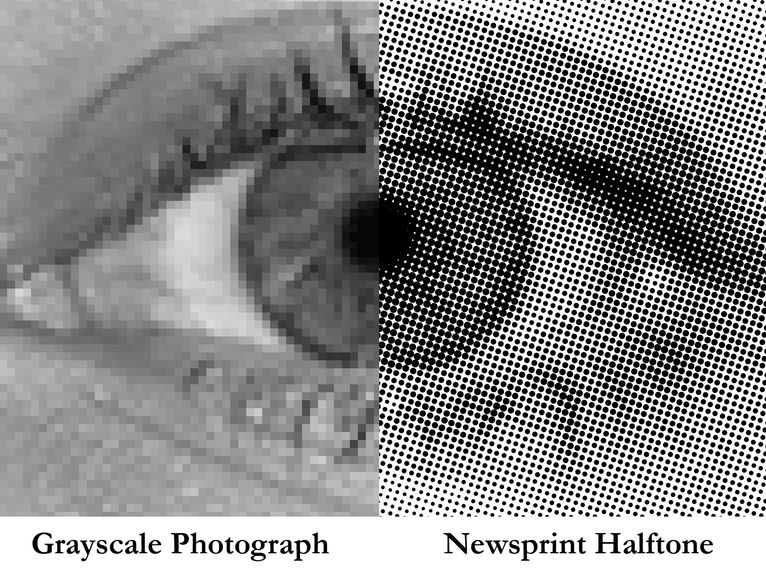
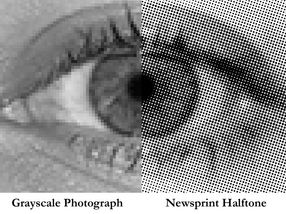
Unlike grayscale photographs, which require several shades of gray to convey gradients (left), halftones (common in newsprint images) can preserve grayscale intensity gradients using only a single color of ink (right). A similar approach was used for processing the image stacks for the 3D printed models described in the paper.
James Weaver/Wyss Institute at Harvard University
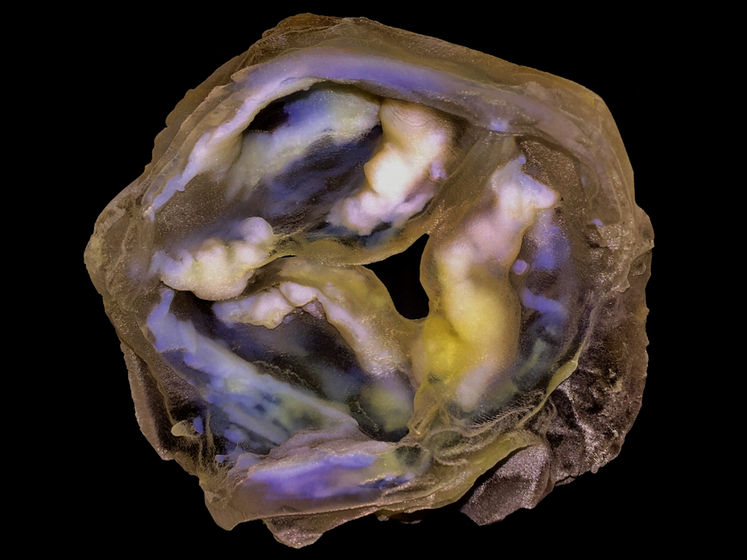
A 3D-printed multi-material model of a calcified heart valve shows hard calcium plaque deposits (white) with fine-scale gradients in mineral density that are impossible to fully capture using conventional biomedical 3D printing approaches.
James Weaver and Ahmed Hosny/Wyss Institute at Harvard University
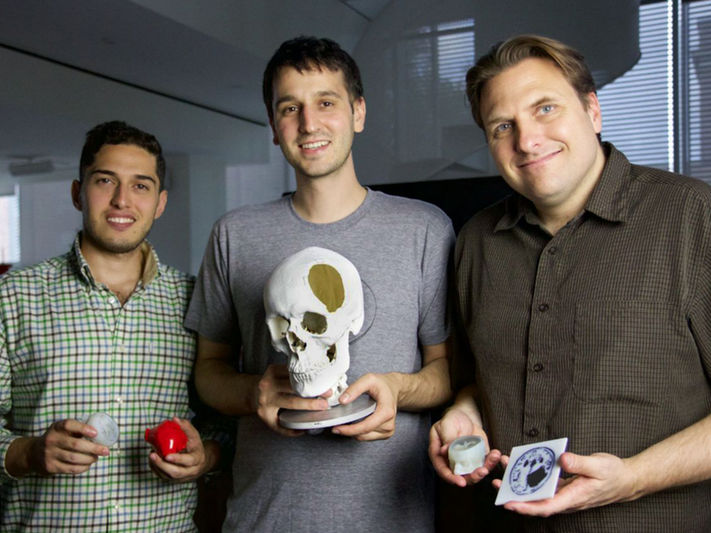
Three of the co-authors of the paper, left to right: Ahmed Hosny holding models of Steven Keating’s tumor, Steven Keating holding a model of his own skull, and James Weaver holding models of Keating’s MRI scan.
Wyss Institute at Harvard University



“It never occurred to us to use this approach for human anatomy until Steve came to us and said, ‘Guys, here’s my data, what can we do?” says Ahmed Hosny, who was a Research Fellow with at the Wyss Institute at the time and is now a machine learning engineer at the Dana-Farber Cancer Institute. The result of that impromptu collaboration – which included scientists worldwide is a new technique that enables highly detailed 3D prints from medical imaging data.
“I nearly jumped out of my chair when I saw what this technology is able to do,” says Beth Ripley, M.D. Ph.D., an Assistant Professor of Radiology at the University of Washington and clinical radiologist at the Seattle VA, and co-author of the paper. “It creates exquisitely detailed 3D-printed medical models with a fraction of the manual labor currently required, making 3D printing more accessible to the medical field as a tool for research and diagnosis.”
MRI and CT scans show slices of the scanned tissue and that is how 3D printing works, slice by slice. This synergy has a drawback as the imaging does not know what part of the body is important for the intended print. This can be solved either manually (called segemntation), which is accurate but extremely time consuming. The other way is automation (called tresholding), which is faster but less accurate. In terms of diagnosis this might erase critical information and maybe lead to misinterpretation.
By using dithered bitmaps, one pixel is changed into a series of pixels of black and white, the scientist were able to combine speed and accuracy. In the 3D printing process these "shaded" pixels are represented by printing material of different colors and therfore keep the information provided by imaging.
The researchers reprinted Keating's brain and also a plaqued heart valve with different materials. This model could be used to explain the influence of rather hard mineral plaques and soft tissue in mechanical tests.
“Our approach not only allows for high levels of detail to be preserved and printed into medical models, but it also saves a tremendous amount of time and money,” says Weaver “Manually segmenting a CT scan of a healthy human foot, with all its internal bone structure, bone marrow, tendons, muscles, soft tissue, and skin, for example, can take more than 30 hours, even by a trained professional – we were able to do it in less than an hour.”
The scientists see that method as an opportunity to get better understanding how different tissues interact. “Right now, it’s just too expensive for hospitals to employ a team of specialists to go in and hand-segment image data sets for 3D printing, except in extremely high-risk or high-profile cases. We’re hoping to change that,” says Hosny.
To be effective the imaging data must not be compressed, as usual today and the access to software and device controls needs to be improved. But the researchers are confident that their achievements present a significant value to the medical community. “I imagine that sometime within the next 5 years, the day could come when any patient that goes into a doctor’s office for a routine or non-routine CT or MRI scan will be able to get a 3D-printed model of their patient-specific data within a few days,” says Weaver.
Steven Keating became an advocate on patients rights to access their imaging data and still surveys his own brain by 3D printing to monitor healing and control relapse of his tumor. “The ability to understand what’s happening inside of you, to actually hold it in your hands and see the effects of treatment, is incredibly empowering,” he says.