Breakthrough: Prospect of blood test for Parkinson’s disease for the first time
A new method reliably detects protein changes in blood that are typical of Parkinson's disease: "The results are really sensational"
Until now, the diagnosis of Parkinson's disease has been based primarily on typical movement disorders such as muscle stiffness, slower movements and shaking. However, the disease starts up to twenty years before it becomes noticeable as a result of these symptoms. To date, there have been neither blood parameters nor imaging examinations to produce a definite diagnosis, let alone early recognition. “This is a dilemma. Of course we would like to detect the disease in its early stages and develop measures to prevent patients from becoming stiff, shaky and slow,” explained Dr Annika Kluge from the “Arbeitsgruppe Früherkennung Parkinson” (working group on the early recognition of Parkinson’s) (led by: Professors Dr Daniela Berg and Dr Eva Schäffer) at the Faculty of Medicine at Kiel University (CAU). This is why lots of working groups around the world are looking for reliable clinically applicable biomarkers for this chronic progressive brain disease.

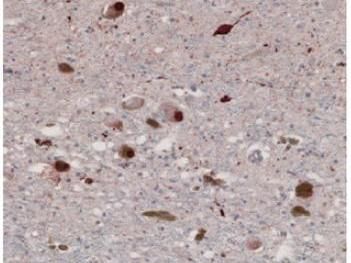
Symbolic image
pixabay.com
The team led by Kluge and biochemist Professor Friederike Zunke, who has since moved to Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), achieved a breakthrough in this respect: “We developed a biochemical blood-based test for the diagnosis of Parkinson's disease. With our procedure, we were able to distinguish the 30 Parkinson’s patients from the 50 control individuals with a very high degree of sensitivity.” The results have now been published in the journal Brain. Also involved alongside the working group in Kiel University's Department of Neurology and Institute of Biochemistry were PD Dr Philipp Arnold (now also at FAU) and Professor Ralph Lucius from the Department of Anatomy. Professor Daniela Berg, director of the Department of Neurology at the University Medical Center Schleswig-Holstein (UKSH), Campus Kiel, stressed that: “The results are really sensational. They form the basis on which a blood test for diagnosing Parkinson's disease can be developed.” She added, however, that the method for doing so requires further development to facilitate a broad-based application. Whether early stages of the diseases can also be detected and whether the test will work for diseases that are similar to Parkinson’s are questions yet to be answered, she added.
Direct detection of the pathogenic protein in the blood
The new method is based on three steps. The first step was to isolate the vesicles of nerve cells in the blood sample. Vesicles are small blisters that are pinched off cells and contain the protein of the original cell. “It is therefore also possible to obtain vesicles from the nervous system by way of a standard blood test. It means I can kind of look into the brain when I examine these vesicles,” explained assistant doctor Annika Kluge from the Department of Neurology at the UKSH, Campus Kiel. The second step was to look specifically for the protein that causes the disease in these isolated nerve cell vesicles. This is a changed form of α-synuclein. This pathogenic form of α-synuclein can be detected through structure-specific antibodies. The young doctor is particularly proud of the third and most significant step of the detection method. “Actually the best part of our work is that we then succeeded in reproducing these misfolded α-synuclein forms of Parkinson’s patients. We have already succeeded in doing that from other tissue samples, but never from vesicles taken from patients’ blood.” This accumulation of pathologically changed α-synuclein is what leads to the destruction of the affected nerve cells and ultimately causes the disease. “The fact that we were able to detect this aggregate formation confirms that pathological α-synuclein forms were present in the sample.”
Original publication
See the theme worlds for related content
Topic world Diagnostics
Diagnostics is at the heart of modern medicine and forms a crucial interface between research and patient care in the biotech and pharmaceutical industries. It not only enables early detection and monitoring of disease, but also plays a central role in individualized medicine by enabling targeted therapies based on an individual's genetic and molecular signature.

Topic world Diagnostics
Diagnostics is at the heart of modern medicine and forms a crucial interface between research and patient care in the biotech and pharmaceutical industries. It not only enables early detection and monitoring of disease, but also plays a central role in individualized medicine by enabling targeted therapies based on an individual's genetic and molecular signature.