Innovative device allows 3-D imaging of the breast with less radiation
Preliminary tests have demonstrated that a new device may enable existing breast cancer imagers to provide up to six times better contrast of tumors in the breast, while maintaining the same or better image quality and halving the radiation dose to patients. The advance is made possible by a new device developed for 3d imaging of the breast by researchers at the Department of Energy's Thomas Jefferson National Accelerator Facility, Dilon Technologies and the University of Florida Department of Biomedical Engineering.
Adding this variable angle slant hole collimator to an existing breast molecular imaging system allows the system to get six times better contrast of cancer lesions in the breast, providing the same or better image quality while also potentially reducing the radiation dose to the patient by half. Technologies developed at DOE's Jefferson Lab for the variable angle slant hole collimator are included in two filings to the US Patent and Trademark Office.
DOE's Jefferson Lab
In breast cancer screening, mammography is the gold standard. But about half of all women who follow standard screening protocol for 10 years will receive a false-positive result that will require additional screening, particularly women who have dense breast tissue. Used in conjunction with mammography, imaging based on nuclear medicine is currently being used as a successful secondary screening alongside mammography to reduce the number of false positive results in women with dense breasts and at higher risk for developing breast cancer.
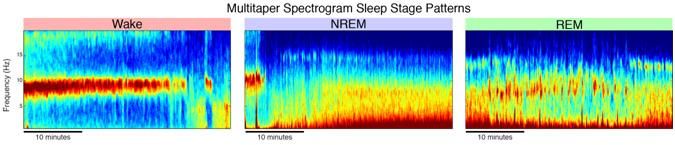
Now, researchers are hoping to improve this imaging technique, known as molecular breast imaging or breast specific gamma imaging, with better image quality and precise location (depth information) within the breast, while reducing the amount of radiation dose to the patient for these procedures.
According to Drew Weisenberger, leader of the Jefferson Lab Radiation Detector and Imaging Group, a new device called a variable angle slant hole collimator provides all of these benefits and more. When used in a molecular breast imager, the device has just demonstrated in early studies to capture 3D molecular breast images at higher resolution than current 2D scans in a format that may be used alongside 3D digital mammograms.
"These results really focus on the breast. We hope to build on this to perhaps improve the imaging of other organs," Weisenberger said. The new device replaces a component in existing molecular breast imagers.
While a mammogram uses X-rays to show the structure of breast tissue, molecular breast imagers show tissue function. For instance, cancer tumors are fast growing, so they gobble up certain compounds more rapidly that healthy tissue. A radiopharmaceutical made of such a compound will quickly accumulate in tumors. A radiotracer attached to the molecule gives off gamma rays, which can be picked up by the molecular breast imager.
"You can image that accumulation external to the breast by using a gamma camera," said Weisenberger.
Current molecular breast imaging systems use a traditional collimator, which is essentially a rectangular plate of dense metal with a grid of holes, to "filter" the gamma rays for the camera. The collimator only allows the system to pick up the gamma rays that come straight out of the breast, through the holes of collimator, and into the imager. This provides for a clear, well-defined image of any cancer tumors.
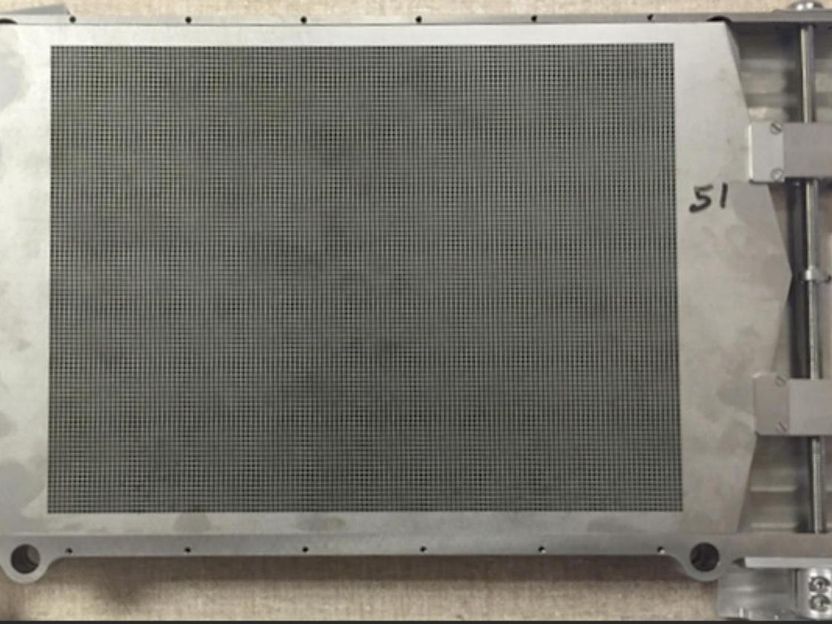
The variable angle slant hole collimator, or VASH collimator, is constructed from a stack of 49 tungsten sheets, each one a quarter of a millimeter thick and containing an identical array of square holes. The sheets are stacked like a deck of cards, with angled edges on two sides. The angle of the array of square holes in the stack can be easily slanted by two small motors that slide the individual sheets by their edges. The result is a systematic varying of the focusing angle of the collimator during the imaging procedure.
"Now, you can get a whole range of angles of projections of the breast without moving the breast or moving the imager. You're able to come in real close, you're able to compress the breast, and you can get a one-to-one comparison to a 3D mammogram," Weisenbeger explained.
In a recent test of the system, the researchers evaluated the spatial resolution and contrast-to-noise ratio in images of a "breast phantom," a plastic mockup of a breast with four beads inside simulating cancer tumors of varying diameter that are marked with a radiotracer. They found that using the VASH collimator with an existing breast molecular imaging system, they could get six times better contrast of tumors in the breast, which could potentially reduce the radiation dose to the patient by half from the current levels, while maintaining the same or better image quality. The test results match a published paper that predicted this performance via a Monte Carlo simulation.
The collimator was built at Jefferson Lab and the test results were analyzed at the University of Florida with funds provided by a Commonwealth Research Commercialization Fund grant from the Commonwealth of Virginia's Center for Innovative Technology, and with matching support provided by Dilon Technologies.