Breaking bad: cancer cell drug addiction solved
cancer cells can become not only resistant but also addicted to the drugs that serve to kill them. A research team led by professor Daniel Peeper from the Netherlands Cancer Institute has now discovered the underlying mechanism, which may guide the development of more rational alternating therapies.
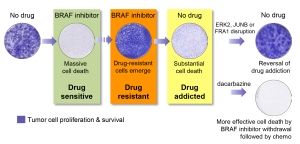
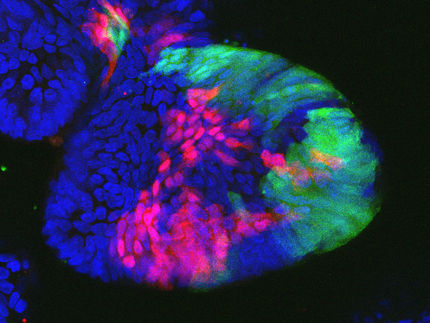
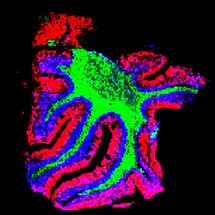
Initially, BRAF mutant melanoma cells are highly susceptible to pharmacologic BRAF inhibition and will massively undergo cell death. Nonetheless, eventually resistant clones often emerge, causing relapse of the disease. Remarkably, such resistant tumor cells can also become addicted to the very drugs that serve to eliminate them: when BRAF inhibition is discontinued, substantial cell death is observed. This study demonstrates that this addiction relies on the activity of the ERK2, JUNB and FRA1 genes, disruption of which breaks drug addiction. As a proof-ofconcept clinical possibility, the researchers show that cell death resulting from drug withdrawal is strongly enhanced if it is immediately followed by a secondary treatment with dacarbazine (chemotherapy).
Netherlands Cancer Institute
Cancers often become resistant to therapy, which is one of the major challenges in patient care. Sometimes however, cancers are not only resistant but also addicted to the very drugs that were supposed to eliminate them. Indeed, studies in patients, animal models and cultured cells have suggested that this dependency can be used against tumors: it turns out that drug-addicted cells massively die when treatment is suddenly stopped. Although this is a potential new avenue to fight cancer, it was not clear how best to exploit this vulnerability in the clinic, because the mechanism of addiction was unknown. Until now.
Breaking addiction
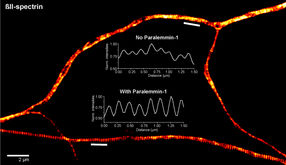
To reveal the mechanism of cancer drug addiction, it is probably best to try to break it, argued group leader Daniel Peeper and his postdoc Xiangjun Kong at the Netherlands Cancer Institute. They started off with melanoma cells that were both resistant and addicted to a treatment based on inhibition of BRAF, a common driver of malignancy. With a popular technique called CRISPR-Cas9 they knocked out all individual genes in the cancer cells’ genome, one by one. Then, they searched for cells carrying a mutation that had broken the addiction. Those were the cells that had managed to survive when treatment was discontinued. All others died. With this strategy, the researchers identified a signaling pathway vital for drug addiction, involving the proteins ERK2, JUNB, and FRA1. Peeper: “Interestingly, all resistant tumor cells we examined used this same drug addiction mechanism irrespective of how they had become resistant.”
“When this pathway is disrupted, cancer cells overcome their drug addiction”, continues Peeper (see illustration). “We have demonstrated this in both cell culture and tumor-bearing mice, and we have indications of the same phenomenon in patients with drug-resistant melanoma. This mechanism was active also in lung cancer cells that were addicted to another drug. This suggests that the pathway we uncovered may be important for various cancer types and treatments.”
Rational alternating treatments
Unfortunately, cancer cells are very flexible and can often reverse their addiction themselves. The new findings may be used to target those addicted cancer cells that fail to die upon stopping the treatment. “Instead of giving addicted cells a break we should probably immediately switch to another treatment”, says Peeper. “Now that we understand how cancer cells can overcome their drug addiction, we have a solid basis for identifying the most effective second treatment for this so-called alternating therapy approach.”
His team already started off with melanoma cells that were addicted to a BRAF-inhibitor. They stopped this treatment and subsequently treated the cells with the chemotherapeutic dacarbazine. This combination of sudden drug withdrawal and a different second treatment turned out to be more effective than just discontinuing the first treatment. Peeper: “This was a proof-of-principle experiment in cultured cells demonstrating how effective these alternating treatments may be. It sets the stage for systematic studies identifying which treatments cooperate best with drug withdrawal for therapy-addicted cancers.”