DNA testing can rapidly solve Legionnaires' disease outbreaks
A DNA test method called polymerase chain reaction (PCR) allowed New York City health officials to identify the source of a Legionnaires' disease outbreak within hours of specimen collection and should be considered in all Legionnaires' outbreak investigations, researchers say in the April issue of the Journal of Environmental Health.
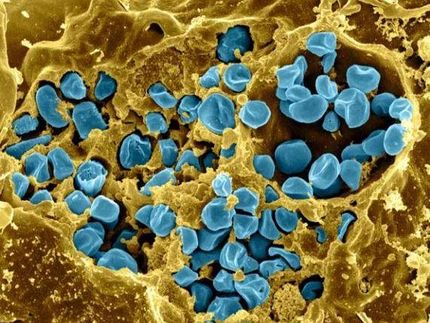
Their study describes the outbreak response and innovative use of PCR rather than the standard method of bacterial culture, which generally takes five to 10 days for a lab to detect the presence of Legionella bacteria, said co-author Christopher Boyd, who led the city's response to the 2014 Legionnaires' outbreak as then-assistant commissioner of environmental sciences and engineering.
"In an outbreak investigation, the ability to identify and mitigate possible sources of exposure is critical to preventing more people from becoming infected. By using PCR, we were able to mitigate risks days earlier than if we had relied on traditional culture methods," said Boyd, who is now general manager of Building Water Health at NSF International, an independent, not-for-profit public health and safety organization.
"Our approach likely helped prevent more people from getting sick, because we were responding much sooner."
Legionnaires' disease, a severe form of pneumonia that occurs from inhaling water droplets from manmade water systems contaminated with Legionella bacteria, is the leading cause of death from waterborne outbreaks. An estimated 8,000 to 18,000 cases a year in the United States require hospitalization.
With a PCR test, fragments of DNA are run through a machine called a thermocycler, which heats and cools the sample repeatedly to produce multiple copies of these DNA fragments, amplifying them for analysis in just a few hours.
Boyd, who co-authored the study with Isaac Benowitz from the U.S. Centers for Disease Control and Prevention (CDC) and other researchers, said while PCR can confirm the presence of Legionella bacteria in a water sample, it cannot reliably tell whether those bacteria are alive or dead (like a bacterial culture can). Only live Legionella bacteria can make people sick.
But since PCR can be completed in one day, Boyd said the test is a valuable tool during a Legionnaires' disease outbreak. In late 2014, he and his team at the New York City Department of Health and Mental Hygiene suspected the outbreak of eight Legionnaires' cases was caused by a building's cooling tower; a PCR water sample from the tower confirmed the presence of Legionella in a single day and the city ordered the cooling tower shut down and disinfected. Days later, results from a bacterial culture of the water came back to show the Legionella bacteria in the cooling tower were, in fact, alive. Further testing showed these bacteria were the cause of the Legionnaires' disease outbreak.
Boyd and his team in New York City would use PCR successfully during a much larger outbreak of Legionnaires' disease in summer 2015 that killed 16 people and sickened more than 100. Another cooling tower was confirmed as the source. The local health department's investigation and response to that outbreak is discussed in another recent study co-authored by Boyd in the journal Public Health Reports.
In addition to PCR testing, Boyd said health departments should have a detailed strategy to deal with Legionnaires' disease outbreaks, including knowing the location of cooling towers. Following the 2015 outbreak, New York City instituted rules for the registration and oversight of all cooling towers.
"Very often in these outbreaks, health officials don't know the source of exposure that is making people sick," Boyd said. "It is critical that public health officials have an inventory of significant sources of risk and detailed response plans to speed the response to an outbreak."
For their part, building owners and managers should have a comprehensive water safety plan for managing pathogens such as Legionella. Boyd and other experts in water safety and public health will discuss these key issues May 9-11 at Legionella Conference 2018 in Baltimore, sponsored by NSF International and the National Science Foundation.
With proper planning and management of building water systems, Legionnaires' disease outbreaks are almost completely preventable, experts say. A recent CDC report, in fact, found that nine in 10 outbreaks can be prevented with more effective water management. But unfortunately, preparing for and managing Legionella in many cases continues to be an afterthought in American society, Boyd said.
"In the United States, we have a very low tolerance for engineered systems to kill people," he said. "We don't allow elevators to fall and we expect fire sprinkler systems to work. So why is it that we continue to accept that failures in the maintenance of engineered water systems are addressed only when public health officials respond to significant increases in Legionnaires' disease cases? There needs to be a paradigm shift among building owners, facility managers and public health officials - these outbreaks are preventable and the trigger for corrective action should no longer be sick and dead people."