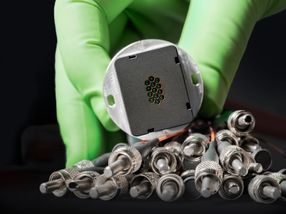
High-risk cardiac devices are safe
Device 'supplement' applications are generally not accompanied by new clinical testing, with implications for patient safety
The Food and Drug Administration (FDA) ensures that high-risk medical devices, such as implantable cardioverter-defibrillators and pacemakers, are safe and effective through its premarket approval (PMA) pathway, during which manufacturers must collect preclinical and clinical data before the device is approved. However, a new study from researchers at Brigham and Women's Hospital (BWH) shows that most cardiac implantable electronic devices (CIEDs) used by physicians today were approved as changes, or "supplements," to existing PMA-approved models, often without the collection of new clinical data. These findings are published in JAMA.
"The original PMA process is widely considered to be the most rigorous regulatory review pathway for device approval in the world," explained Aaron Kesselheim, MD, JD, MPH, assistant professor of medicine in the Division of Pharmacoepidemiology and Pharmacoeconomics at BWH, and senior investigator of this study. "However, we found that many CIED models currently used by clinicians in the United States were approved via the PMA supplement process, not as original PMAs. Key cardiac devices recalled in recent years—such as the St. Jude Medical Riata and Medtronic Sprint Fidelis defibrillator leads—were approved through the PMA supplement process."
Supplements to existing high-risk cardiac devices may include major or minor design changes, as well as routine changes in labeling, materials or packaging. The researchers used the FDA's PMA database to review CIEDs approved from 1979 through 2012. For each supplement, they collected the date approved, type of supplement, and the nature of the changes. They then calculated the number of supplements approved per PMA and analyzed trends in the different supplement regulatory categories over time. For supplements indicating major design changes from 2010-2012, they identified how often additional clinical data were collected.
They found that since the first CIED was approved via PMA in 1979, the FDA has authorized 5829 supplements for 77 PMA applications, translating to an average of 50 supplements per PMA. Over a third of supplements involved a change to a device's design or materials, and in the majority of these cases the FDA deemed that new clinical data were not necessary for approval. PMA applications remained active via successive supplements over a median period of 15 years, with 79% of the 77 PMAs approved during the study still being the subject of at least 1 supplement in 2012.
"We found that most new cardiac implantable electronic device models currently in use were deemed deemed safe and effective without requiring new clinical data," said Benjamin Rome, a Harvard Medical School student and lead author of the study. Small changes made in each successive supplement add up over time and can lead to a device that looks nothing like the original product on which the supplement's approval was based. These small changes may also have important implications for patient safety, as evidenced by the Riata and Sprint Fidelis recalls.
"The PMA supplement process allows manufactures to easily update devices, which means that useful technological advances can be rapidly integrated in clinical care," explains Daniel Kramer, MD, a cardiac electrophysiologist at the Beth Israel Deaconess Medical Center and co-author on the study. "However, a large number of the cardiac devices implanted in patients are approved as PMA supplements, and clinicians and patients should consider the strengths and limitations of the PMA supplement approval process when making decisions about the use of these high-risk devices."
The researchers note that approval of high-risk devices as PMA supplements reinforces the need to perform rigorous post-market surveillance. They hope that their results will encourage the clinical community to conduct more comparative effectiveness studies to guide clinicians who need to choose among many similar device models.
Organizations
Other news from the department science

Get the analytics and lab tech industry in your inbox
From now on, don't miss a thing: Our newsletter for analytics and lab technology brings you up to date every Tuesday. The latest industry news, product highlights and innovations - compact and easy to understand in your inbox. Researched by us so you don't have to.


![[Fe]-hydrogenase catalysis visualized using para-hydrogen-enhanced nuclear magnetic resonance spectroscopy](https://img.chemie.de/Portal/News/675fd46b9b54f_sBuG8s4sS.png?tr=w-712,h-534,cm-extract,x-0,y-16:n-xl)