MRI Guidance Shows Promise in Delivering Stem Cell Therapies
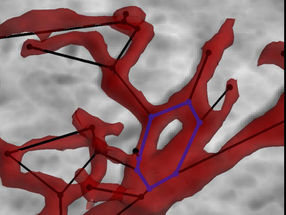
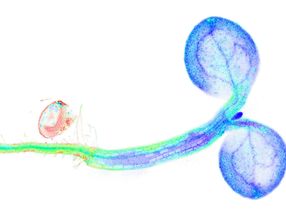
Working with animals, a team of scientists reports it has delivered stem cells to the brain with unprecedented precision by threading a catheter through an artery and infusing the cells under real-time MRI guidance.
In a description of the work they express hope that the tests in anesthetized dogs and pigs are a step toward human trials of a technique to treat Parkinson’s disease, stroke, and other brain damaging disorders.
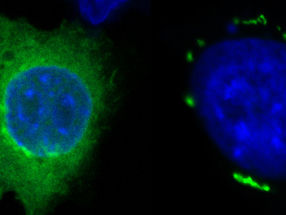
“Although stem cell-based therapies seem very promising, we’ve seen many clinical trials fail. In our view, what’s needed are tools to precisely target and deliver stem cells to larger areas of the brain,” says Piotr Walczak, M.D., Ph.D., associate professor of radiology at the Johns Hopkins University School of Medicine’s Institute for Cell Engineering. The therapeutic promise of human stem cells is derived from their ability to develop into any kind of cell and, in theory, regenerate injured or diseased tissues ranging from the insulin-making islet cells of the pancreas that are lost in type 1 diabetes to the dopamine-producing brain cells that die off in Parkinson’s disease.
Ten years ago, Shinya Yamanaka’s research group in Japan raised hopes further when it developed a technique for “resetting” mature cells, such as skin cells, to become so-called induced pluripotent stem cells. That gave researchers an alternative to embryonic stem cells that could allow the creation of therapeutic stem cells that matched the genetic makeup of each patient, greatly reducing the chances of cell rejection after they were infused or transplanted. But while induced pluripotent stem cells have enabled great strides forward in research, Walczak says they are not yet approved for any treatment, and barriers to success remain.
In a bid to address once such barrier – how to get the cells exactly where needed and no place else – Walczak and his colleague Miroslaw Janowski, M.D., Ph.D., assistant professor of radiology, sought a way around strategies that require physicians to puncture patients’ skulls or inject them intravenously. The former, Walczak says, is not only unpleasant, but also only allows delivery of stem cells to one limited place in the brain. In contrast, injecting cells intravenously scatters the cells throughout the body, with few likely to land where they’re most needed, says Walczak.
“Our idea was to do something in between,” says Janowski, using intra-arterial injection, which involves threading a catheter, or hollow tube, into a blood vessel, usually in a leg, and guiding it to a vessel in a hard-to-reach spot like the brain. The technique currently is used mainly to repair large vessels in the brain, says Janowski, but the research team hoped it might also be used to get stem cells to the exact place where they were needed. To do that, they would need a way of monitoring the catheter placement and movement of implanted cells in real time.
Walczak and Janowski teamed with colleagues including Monica Pearl, M.D., an associate professor of radiology practicing in the Division of Interventional Neuroradiology, who specializes in intra-arterial procedures. Usually the procedure is performed using an X-ray image as a guide, but that approach ruled out watching injected stem cells’ movements and making adjustments in real time.
In their experiments, after placing the catheter under X-ray guidance, they transferred anesthetized dog and pig subjects to an MRI machine, where images were taken every few seconds throughout the procedure. Once the catheter was in the brain, Pearl pre-injected small amounts of a harmless contrast agent that included iron oxide and could be detected on the MRI. “By using MRI to see in real time where the contrast agent went, we could predict where injected stem cells would go and make adjustments to the catheter placement, if needed,” says Janowski. Adds Jeff Bulte, Ph.D., a professor of radiology who participated in the study, “It’s like having GPS guidance in your car to help you stay on the right route, instead of only finding out you’re lost when you arrive at the wrong place.”
The team then injected both small stem cells (glial progenitor cells from the brain) and large mesenchymal stem cells from bone marrow into the animals under MRI, and found that in both cases, the pre-injected contrast agent and MRI allowed them to accurately predict where the cells would end up. They could also tell whether clumps of cells were forming in arteries and, if so, possibly intervene to avoid letting the clumps grow large enough to cut off blood flow and pose a danger. “If further research confirms our progress, we think this procedure could be a big step forward in precision medicine, allowing doctors to deliver stem cells or medications exactly where they’re needed for each patient,” says Walczak. The research team is planning to test the procedure in animals as a treatment for stroke and cancer, delivering both medications and stem cells while the catheter is in place.
Original publication
Piotr Walczak, Joanna Wojtkiewicz, Adam Nowakowski, Aleksandra Habich, Piotr Holak, Jiadi Xu, Zbigniew Adamiak, Moussa Chehade, Monica S Pearl, Philippe Gailloud, Barbara Lukomska, Wojciech Maksymowicz, Jeff WM Bulte, and Miroslaw Janowski; "Real-time MRI for precise and predictable intra-arterial stem cell delivery to the central nervous system"; J Cereb Blood Flow Metab; 2016


















![[Fe]-hydrogenase catalysis visualized using para-hydrogen-enhanced nuclear magnetic resonance spectroscopy](https://img.chemie.de/Portal/News/675fd46b9b54f_sBuG8s4sS.png?tr=w-712,h-534,cm-extract,x-0,y-16:n-xl)