Non-Invasive Imaging Tools May Help Unravel Mechanisms of Prenatal Drug Damage
Technique may also help assess, improve effectiveness of pain medication following fetal surgery
Scientists at the U.S. Department of Energy's Brookhaven National Laboratory demonstrate a new way to assess the potentially damaging effects of prenatal drug exposure -- a technique that could also be used to monitor a fetus's response to therapeutic drugs -- using sophisticated, non-invasive medical-imaging tools. The scientists used magnetic resonance imaging (MRI) combined with positron emission tomography (PET) to track the uptake and distribution of trace amounts of cocaine in pregnant monkeys and found significant differences in where and how fast the drug accumulates in maternal and fetal organs.
"Understanding how drugs are transferred between a mother and her fetus during pregnancy may help us unravel the mechanisms of the drug's damaging effects on unborn children," said Helene Benveniste, Chair of Brookhaven's Medical Department and lead author of the paper, which appears in the February 2005 issue of the Journal of Nuclear Medicine. "While studies that follow human drug abusers and their children over decades provide valuable information, animal studies can more quickly provide clues to the underlying mechanisms of damage and suggest ways to test new treatment or prevention strategies," she said.
The imaging tools could also be used to assess the effects of therapeutic drugs, for example, synthetic narcotics administered to pregnant women following surgical procedures performed on fetuses in utero. "Following such surgeries, which are becoming more common to correct congenital malformations, the mother is treated with narcotics for pain - and anesthesiologists are relying on the mother transferring the pain medication to the fetus via the placenta. But we actually do not know if what we give is sufficient to 'satisfy' the pain level of the fetus," said Benveniste, who is also a professor of anesthesiology at Stony Brook University.
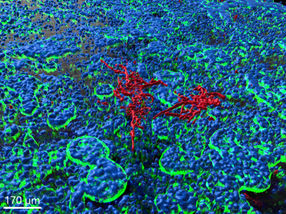
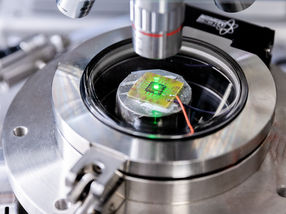
Though other scientists have attempted to use PET to non-invasively monitor maternal-fetal drug exchange and pharmacokinetics (how quickly a drug is taken up and distributed among the body's organs), the PET technique alone did not provide adequate anatomical detail of the tiny fetal organs. The current study combined PET with high-resolution magnetic resonance imaging (MRI) - complementary non-invasive techniques available at Brookhaven Lab's Center for Translational Neuroimaging - to track cocaine pharmacokinetics down to the level of the placenta and individual regions of the fetal brain.
"The MRI images, which have the necessary detail, served as a high-resolution anatomical template onto which we 'overlayed' the PET pharmacokinetic data using sophisticated computer techniques," Benveniste said. "The resulting images gave us the best of both worlds and allowed us to look at cocaine uptake and distribution in the mother and fetus simultaneously."
The animals were anesthetized prior to scanning. MRI scans were performed first, followed by PET. For the PET study, each animal was injected with a trace quantity of cocaine - less than 10 micrograms, which is not enough to cause pharmacological effects. The injected cocaine had previously been "labeled," or "tagged," with a short-lived radioactive form of carbon (carbon-11). This "radiotracer" emits a signal that is picked up by the PET scanner, which takes "snapshots" of the tracer's location over time to show how much and how quickly the cocaine (and/or the metabolic byproducts that retain the carbon-11) enters and clears the various organs. The radiotracer decays and completely clears from the animal's body in about two hours. After the procedure, the animals were returned to their social colony to deliver their offspring.
The combined images show that cocaine and/or its labeled metabolites readily cross the placenta. But the cocaine uptake distribution pattern observed in the fetus was very different from that of the mother. For example, mothers showed rapid uptake and clearance of the drug in the heart, kidneys, and lungs, with slower uptake in the liver and brain. In the fetus, cocaine accumulated at the highest levels in the liver (due to the unique anatomy of fetal circulation) and to a lesser extent in the brain.
"While the uptake of the tracer into the fetal brain is lower and slower than in the mother's brain, a measurable quantity of cocaine and/or its labeled metabolites does accumulate in the fetal brain, particularly in the striatum, where cocaine is known to bind to cell-surface receptors that result in a euphoric response," Benveniste said.
The high uptake of radiolabeled cocaine in the placenta is also particularly relevant, the researchers said, because cocaine is known to constrict blood vessels in the placenta. It may be that this constriction of placental blood flow is one of the mechanisms underlying the harmful effects of cocaine exposure during pregnancy.
The research was funded by the Office of Biological and Environmental Research within the U.S. Department of Energy's Office of Science and the National Institute on Drug Abuse. The monkeys were obtained from the Primate Laboratory, Department of Psychiatry, State University of New York, Downstate.
PET and MRI are a direct outgrowth of the Department of Energy's long-standing investment in basic physics research. Through work on accelerators designed to answer questions about the fundamental nature of matter and energy, pioneering DOE scientists understood and realized the potential to develop these miraculous tools for the diagnosis and treatment of disease. The ongoing research using these tools to investigate drug addiction and other diseases of the brain is a prime example of how our national laboratories bring together the expertise of chemists, physicists, and medical professionals to address questions of profound significance for society.